We have strong links with the Nuffield Department of Surgery at the John Radcliffe Hospital, and we work closely with the Donor Transplant Coordinators.
Procedures we carry out
Kidney transplantation
Kidney transplantation is performed using kidneys retrieved from either deceased ('cadaveric') or live organ donors. The transplant procedure may be performed on patients with kidney failure due to a large variety of causes, but the most common are diabetes, inherited polycystic kidney disease, glomerulonephritis and pyelonephritis.
About 100 patients a year receive a kidney transplant at Oxford, and the region serves stretches between Swindon in the south, Gloucester in the west, High Wycombe in the east and Banbury in the north.
Kidney Transplant Co-ordinators
For further information on kidney transplantation, please contact:
- Clare Snelgrove: 01865 228660
- Jen Day: 01865 228661
Living Donor Team
Living Donor Team - Oxford University Hospitals
Pancreas transplantation
Pancreas transplantation is a procedure usually performed to treat patients who have a failure of their pancreas to produce insulin, most often due to 'type 1' diabetes, where the insulin secreting cells which are normally scattered throughout the pancreas in clusters called 'islets' have been destroyed by their own immune system - an autoimmune disease.
Pancreas transplantation is performed using pancreases retrieved from cadaveric organs, and is carried out in a similar way to a kidney transplant, by joining the blood vessels to those of the patient receiving the transplant.
Most patients receive their pancreas at the same time as a kidney transplant, a procedure called 'simultaneous kidney/pancreas graft' (SPK). This is usually the best option for patients who have kidney failure caused by long-term diabetes. Some diabetic patients who have had a previous kidney transplant then go on later to have a pancreas transplant ('pancreas after kidney (PAK)'). Occasionally patients who have found severe difficulties controlling their diabetes and have early signs of kidney failure are transplanted with a 'pancreas transplant alone' (PTA).
Oxford Transplant Centre is one of seven national centres performing pancreas transplantation. Patients come from as far afield as Portsmouth, Bristol, Dorset and London.
Pancreas Transplant Co-ordinator
For further information on pancreas transplantation, please contact:
Simon Northover: 01865 228658
Pancreatic islet transplantation
This is a procedure which is considered experimental in Oxford, as the clinical protocols and necessary laboratory procedures are still in the process of development. However, in a number of centres around the world the procedure is now in routine clinical practice, and it is hoped this will be the case in Oxford in the near future.
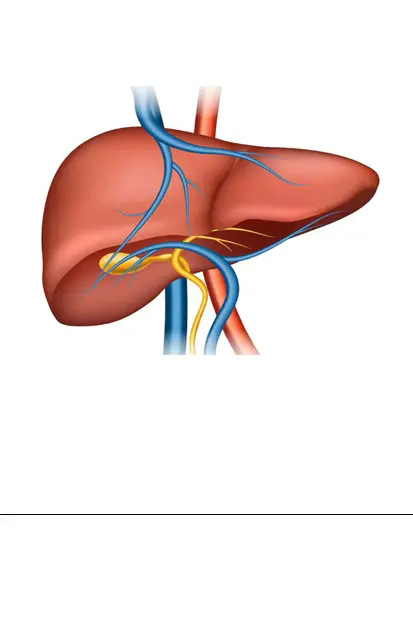
Islet transplantation in patients with diabetes involves separating out the insulin-producing islet tissue from within the pancreas and transplanting the islets as a simple injection into the liver, where they develop their own blood supply and produce insulin as required.
The aim is to replace pancreas transplantation with an islet graft, but the process is not yet advanced enough to allow single donor transplantation. However, certain diabetic patients, who have major problems with hypoglycaemia and contraindications to vascularised pancreas transplantation, can be considerably improved by islet transplantation.
Islet Transplant Co-ordinator
For further information on pancreatic islet transplantation please contact:
Simon Northover: 01865 228658
Intestinal transplantation / small bowel transplant
Intestinal transplantation is an operation to replace diseased or shortened bowel with the healthy bowel from a donor. Small bowel transplant may be an option for those individuals whose bowel no longer works and who are dependent on being fed via total parenteral nutrition (TPN) - liquid feed via a vein into the body.
It may become necessary for some individuals on TPN to consider a small bowel transplant if their liver shows signs of damage from the TPN, or if they have problems with intravenous line infections, or even lose line access.
Bowel transplants have been performed in Oxford since 2008 and internationally since the 1960s. Following small bowel transplant patients can be weaned off TPN on to a normal oral diet.
A multidisciplinary team approach is paramount in the success of the transplant. Patients are rigorously assessed by a multidisciplinary team before being deemed fit for the operation.
Small bowel transplantation is a complicated and difficult operation that comes with risks. In the past there were high rates of rejection of the new organ. In recent times, with the development of medicines to manage rejection, immunosuppression and greater experience, survival rates are improving.
Intestinal Transplant Co-ordinator
For further information on intestinal transplantation / small bowel transplant please contact:
Kim Corbey: 01865 228671
Total Pancreatectomy with Islet Autotransplantation (TPIAT)
Oxford Transplant Centre is one of only four NHS trusts in England offering Total Pancreatectomy with Islet Autotransplantation (TPIAT).
Inflammation of the pancreas causes severe pain. In a small number of patients, long-term pancreatitis is so disabling as to require surgical removal of the pancreas (total pancreatectomy or TP). This controls or abolishes the pain, but it also removes all the insulin producing cells of the body, resulting in a very severe form of diabetes.
The newly developed technique of islet autotransplant (IAT) involves separating the insulin-producing islet cells from the patient's own pancreas in a laboratory, after the surgeon has performed the pancreatectomy, and infusing them back into the patient's body, with an aim to greatly improve the inevitable diabetes of total pancreatectomy.
This procedure has made it possible for many people to return to their normal activities without pain.
Patient assessment, pancreatectomy, islet isolation and ongoing care all demand great expertise which is provided by our multidisciplinary team in Oxford.
TPIAT CNS
For further information on TPIAT please contact:
Jenny Fox: 01865 228662
Transplant Nurse Practitioners (all organ transplant follow-up)
The Transplant Nurse Practitioners are a team of five nurses looking after all transplant recipients who receive their transplant in Oxford.
They carry out regular clinics and provide a telephone advice line during office hours.
Lead Transplant Nurse Practitioners
For further information on transplant follow-up please contact:
Ali Smith or Abigail Fullard: 01865 228658
Transplant Immunology Laboratory Handbook
Transplant Immunology & Immunogenetics Laboratory Handbook (pdf, 614 KB)
Find us and contact us
We are on Level 1, Surgery and Diagnostics Centre, Churchill Hospital
Outpatient clinic desk
Tel: 01865 225355 / 225356
Transplant Ward (enquiries regarding inpatients only)
Tel: 01865 235010 / 235112
Inpatients' mobile phone (to speak to an inpatient)
Tel: 01865 226106
Quality in Organ Donation (QUOD)
The Quality in Organ Donation (QUOD) initiative is a nationwide programme which aims to identify pathways of injury and repair in donor organs.